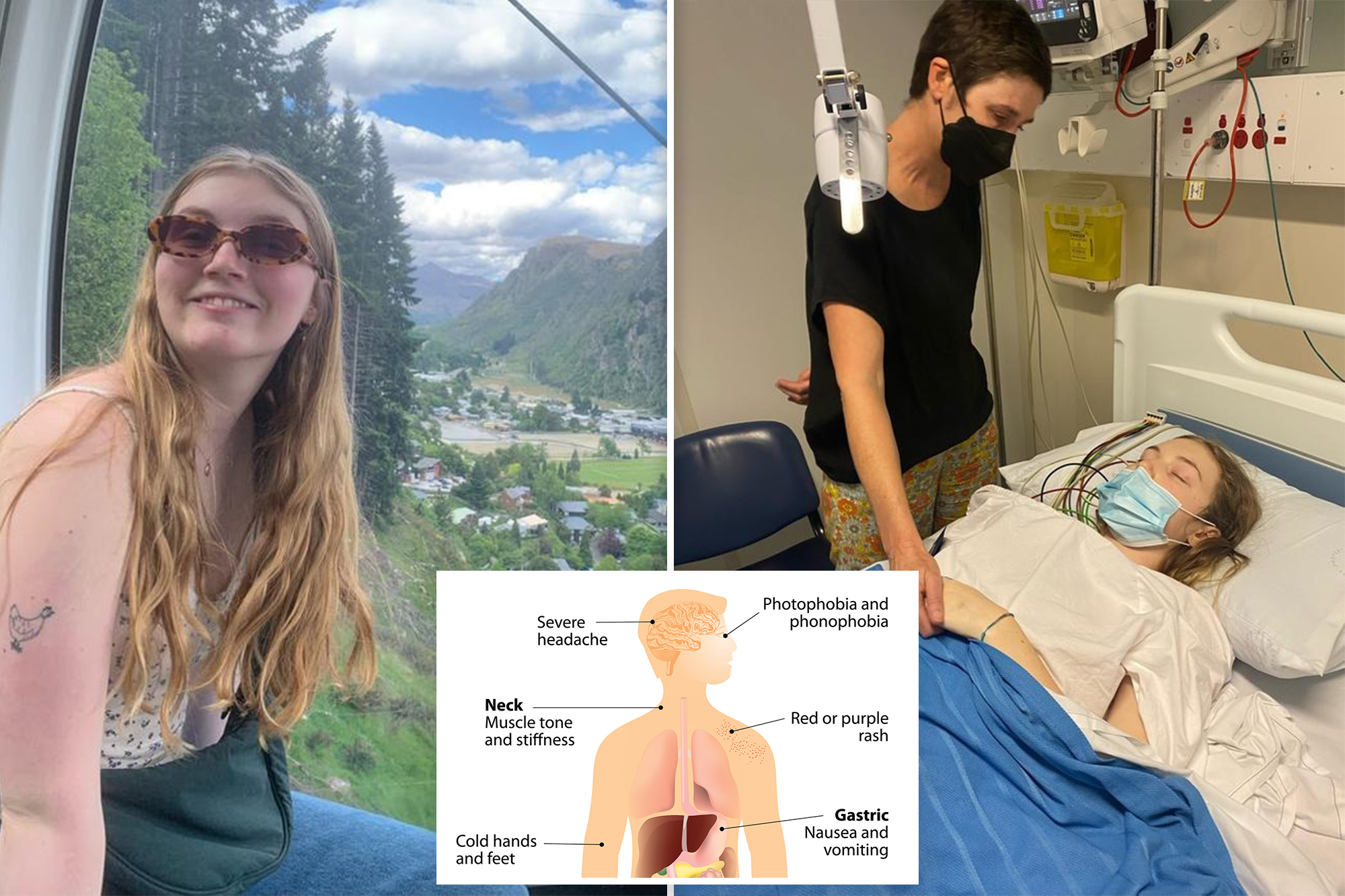
Claudia Gill was only 18 when she came within hours of death as meningococcal attacked her body.
Two years on, the university student is warning everyone to beware of the symptoms.
After coming home from an extended holiday in Queensland, the New South Wales woman was struck with fatigue, her ears were very sensitive to sound and a ringing echoed in her head.
Her neck stiffened, she was vomiting and fainted.
The young woman was rushed to hospital and doctors figured out she had a potentially deadly meningococcal B bacterial infection.
Doctors told her had she arrived at hospital any later there was a good chance she would have died.
Her recovery took five nights in hospital, weeks of rest and slowly getting back into work and study. Two years on Ms. Gill gets more regular and intense headaches.
Once she was out of hospital she wanted to find the community of people who have had the disease, and learn about what attacked her body.
From there Gill started speaking with community and advocacy groups, and realised she would be a good test case for advocacy about the disease.
“It comes on so quickly … it was pretty scary,” Ms Gill said.
She wants people to be aware of the symptoms so they can act quickly should they suspect an infection.
Gill only got a minor rash, which tends to be a later symptom often associated with meningococcal.
The rash followed the progressively mounting light and sound sensitivity, stiff neck, nausea, stiff back, vomiting, and then a fully-stiff body and headaches.
“If I had the rash earlier then we would have acted earlier. But that’s why it’s so important to know all the symptoms,” she said.
Meningococcal is a type of bacteria which can enter your bloodstream and cause blood poisoning.
Vaccinations against the A, C, W and Y variants are free in Australia for newborns, 14-16-year-olds and people with asplenia and hyposplenia, complement deficiency and those receiving treatment with eculizumab.
Gill was struck with meningococcal B. The vaccine for this is free for people with the above immune conditions, as well as Aboriginal and Torres Strait Islander newborns.
Meningococcal deaths in Australia make news because of the widespread vaccine coverage we have, but also the rapid onset of the disease.
Last week a West Australian adult died from the disease, and two others were hospital; the cases were not linked but was the first fatality in the state since 2020.
Gill studies in Newcastle, but is originally from Wollongong.
It was in Wollongong in late 2022 that 23-year-old Brayden Chater became brain dead and died of meningococcal B. His condition deteriorated rapidly in the space of 24 hours, from feeling as if he had just a fever to convulsions and being unresponsive.
Doctors could not tell Gill where she contracted the bacteria.
Australia wide there were 143 lab confirmed cases of all meningococcal variants in 2023. Infections were most common in toddlers and 15 to 19-year-olds.
New South Wales had the most cases (36) last year, but the Northern Territory and South Australia had the highest occurrence per capita, about one case per 100,000 people.
So far in 2024 there have been 31 confirmed cases, with the most being South Australia’s total of nine.














